Botanical and Natural Treatments for Thyroid Dysfunction
Please stop blaming the thyroid gland for thyroid dysfunction. A recent book title asks: “Is your Thyroid Making You Ill?” (2). This is an example of the continuing deionization of the human thyroid gland. We make our thyroid glands sick, not the other way around. A particular thyroid gland is at the mercy of its host human for food, shelter, and a thyrosupportive environment. Rather, a person’s behavior contributes significantly to any subsequent thyroid gland dysfunction. Please engage the thyroid gland as an obligate ally rather than a mass of misbehaving errant tissue, which must be disciplined with medications, radiation ablation, or surgical removal. The thyroid gland is probably usually doing its best to respond to events and demands.
What follows are actions I have recommended for gently modifying thyroid gland activities in referred patients; first for hyperthyroidism and secondly hypothyroidism.
HYPERTHYROIDISM
1. In non-acute hyperthyroidism I recommend iodine starvation as a simplistic approach to quelling thyroid hormone production. T4 and T3 thyroid hormone production is completely iodine dependent. Less iodine from dietary and topical sources means less iodine for MIT, DIT, T3 and T4 production. The human body usually responds to severely reduced iodine intake by becoming extremely iodine conservative, reducing iodine excretion and increasing iodine recycling.
The practical steps to encourage patient compliance are:
- a. Remove iodized salt from the household and, control visits to restaurants and households where iodized salt is used. Iodized salt is usually not used in salted snack foods. Canned, frozen, dried foods may or may not contain iodized salt.
- b. Reduce or eliminate all seafood: fish, shellfish (clams, oysters mussels, true scallops) crustaceans (shrimp, crabs, lobster), echinoderms (sea urchins, sea cucumbers), cephalopods (octopus, cuttlefish, squid), and all seaweeds from diet.
- c. Reduce or eliminate all milk-based dairy products. Whey and milk solids in any prepared food will likely be unlabeled sources of iodine. Most milk and milk products originate in milk factories where cows’ teats and udders are washed before and/ or after each milking with a strong iodine solution, which can drip into the milking apparatus. Iodine is never listed as an ingredient of milk and milk products; this includes so-called organic milk. Manure-caked teats must be washed and disinfected somehow, even organic teats. (Butterfat contains very little iodine unless salted with iodized salt.) One curiosity is the occasional listing of cacao beans as a source of iodine, when the likely source of the iodine is from milk in processed chocolate.
- d. Reduce or eliminate all commercial flour products: breads, crackers, cookies, pasta unless labeled as iodine-free. Iodine is used as a dough conditioner and antimicrobial; it is never listed as an ingredient.
- e. Eliminate all red meat and red meat products, especially blood products (blood pudding and sausages). I do not know if globulin-bound thyroid hormones in red meat are destroyed by cooking. Rare or raw red meats will have thyroid hormones available for human absorption when eaten.
- f. For a somewhat different view of the relationship between dietary iodine intake and thyroid pathology see: www.optimox.com (10)
2. Increase consumption of raw, leafy green brassicas. Kale, cabbage, collard greens, mustard greens, rocket, cress, turnip greens all have constituents causing a mild thyrostatic effect by reducing iodine uptake. Excess raw cabbage consumption (R. Weiss’ “one-sided cabbage diet”) (5) can induce goiter.
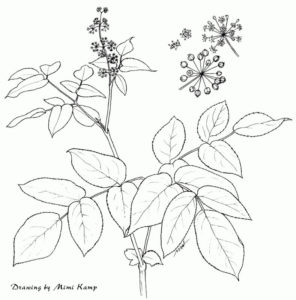
3. Use of one or more of three thyrosuppressive mints; Lemon Balm (Melissa officinalis), Bugleweed (Lycopus spp.), and Motherwort (Leonurus cardiaca). These can be used as fresh plant, freeze-dried capsules, and/or tinctures (6). Fresh material used as a green drink or in tincture must be finely chopped prior to use to release the active constituents, which then can bind directly to TSH-specific receptor docking sites on thyroid cell surfaces. (Thanks to Kerry Bone, plant chemist). Freshly juiced Lemon Balm, an ounce or two, daily, has been very effective in moderate chronic Graves’ non-responsive to tinctures. A few drops of tincture under the tongue can be effective in a few hours; for other patients, several weeks may pass before any obvious symptom improvement.
4. In immune-driven Graves’ hyperthyroidism, immune tonics, not stimulants, are recommended. A mild immune tonic can be prepared as a strong, slowly cooked broth made with finely chopped or powdered dried Ganoderma mushroom (G. lucidum. G. applanatum, G. tsugae) also known as Reishi. I use a crock-pot with 4-8 hours of cooking at low heat. Tinctures and capsules of Ganoderma spp. and Eleutherococcus are also helpful.
5. Sourcing the hyperthyroidism: what is the patient’s role in generating the pathology? Robert Graves, the Irish physician who first clearly described the syndrome bearing his name, wrote in an 1850’s paper that many if not most of his patients suffered from severe ”vexations”; a wise observation. Today we might say most Graves’ patients are burdened with excessive stressors, particularly stressors perceived as unpleasant, persistent and intractably irresolvable. This certainly has been my continued observation. Often, a particular event or events cluster is clearly associated with sudden onset Graves’. Stressor mitigation or resolution may reduce or resolve Graves’. A troubling question: what might be the secondary gain to the patient from maintaining the pathology? Is the immune-modulated hyperthyroidism a natural response to increased life demands? Rather than pathology, hyperthyroidism may be an attempt to increase resources available to cope with increased stressor loads. On the other hand, it may be that the Graves’ is actually generating the sense of too much stress, rather than the stress precipitating the Graves’ condition.
6. Even though soy isoflavones are thyrodisruptive, I caution against their use therapeutically to control thyroid activity.
HYPOTHYROIDISM
Hypothyroidism can be induced by many factors, external and internal. For many years I have believed some cases of hypothyroidism to be health- positive responses to ridiculous life situations. The body’s refusal to devote energy to health-negative activities may be forcing an involuntary inability to cope with life’s demands. Intervention would then be an insult to body wisdom. Other cases, however, seemed to be caused by external factors, rather than glandular hypothyroidism. Some patients diagnosed as hypothyroid from superficial clinical observations were actually suffering from chronic carbon monoxide poisoning from unvented gas flames at home and/or leaky automobile exhaust systems, especially in the American Northeast. Others were chronically sleep-deprived. Correction of the non-thyroid problems seemed to resolve the symptoms thought to indicate hypothyroidism.
I try to encourage everyone to lead a thyrosupportive lifestyle:
1. Adequate dietary iodine: iodine is essential for T4 and T3 and hence all vertebrate life. No land plants seem to require iodine and few beyond the seashore have more than tiny amounts. All of the animals we regularly eat have significant amounts of iodine, especially red-blooded animals and seafood. All seaweeds are rich in iodine. Iodized salt is a reliable dietary iodine source. The intense fatigue experienced by some vegans (iodine occurs in both eggs and dairy) may be iodine-deficiency hypothyroidism (check for goiter). Dairy products contain iodine (see above); baked goods may. Commercial sea salt is not an adequate source of dietary iodine. Salted snacks are usually not salted with iodized salt for reasons of economy.
2. Reduce or eliminate exposure to any and all iodine displacers. The other halogens in various forms can displace or interfere with iodine metabolism. These are Fluorine (toothpaste, water supplies), Chlorine (water supplies and cleaning agents), and Bromine (industrial stack emissions, pesticides in food and spas, preservatives and conditioners). Although these agents may not actually cause hypothyroidism, they add an unexpected burden to thyroid metabolism; most of them did not occur naturally in the thyroid gland’s developmental past, precluding protective mechanisms against them.
3. Reduce or eliminate thyrosuppressive and thyrodisruptive foods such as raw leafy brassicas and soy products.
4. Reduce or eliminate thyrodisruptive medications: aspirin, HRT, warfarin and other anticlotting drugs, many antidepressants, and steroids, particularly cortisone and prednisone.
5. Thyroxine, T4, is converted to T3 by several selenodiodinases (1). Selenium deficiency may result in hypothyroid symptoms. Ensure adequate dietary selenium. Recent work suggests that selenium supplementation may control or modulate autoimmune thyroid disease (5). No plants seem to require selenium although they do extract it from soils. Avoid excess selenium. Excess selenium seems to quench itself in enzymes. Mercury, cadmium and perhaps other heavy metals may quench selenium in the selenodiodinases. Check for metal poisoning in cases where T4 production is okay but T3 levels are low with accompanying symptoms of hypothyroidism. Reduce or eliminate home and workplace exposure to mercury and cadmium.
6. If blood thyroid hormone levels are within or near normal ranges but symptoms indicate hypothyroidism, suspect incomplete body mineralization. T4 and T3 are middle-management directive molecules, carrying orders. Downstream enzymes need to do the work to actualize thyroid hormone-mediated orders. Most of those enzymes require metallic cations. Deficiencies of one or more enzymatic cations could manifest as hypothyroid symptoms. Use a mineral supplement or high-mineral powdered kelp (not tablets), added to regular food as a salt replacement. Also, improve diet to include mostly organic whole foods and seaweeds.
7. Natural sources of thyroid hormone:
a. Fucus contains di-iodotyrosine (DIT), the basic building block of T4 (two DIT are condensed in an esterification reaction by thyroid peroxidase in thyroid follicles to produce T4) (3,6). If blood thyroid hormone levels are low and TSH is modestly elevated (5.0-10.0) consider natural supplementation with powdered Fucus spp. seaweed, (bladderwrack). Take up to 5grams/day, one hour before a regular meal. Positive results may develop within several days or weeks. Some patients with functioning thyroid glands on low dosages of thyroid hormone medication have successfully used Fucus seaweed to either replace or wean themselves from T4 medications. In one patient with 17-yr Hashimoto’s thyroiditis, Fucus was used for two years to successfully replace T4 medication with both a lowering of TSH after 2-3 months and a reduction in thyroid gland swelling. CAUTION!! Fucus seaweed powder cannot replace T4 medication taken by those patients who have had a complete thyroidectomy or radiation ablation of their thyroid gland. DIT is weakly active as a thyroid hormone but cannot replace T4 or T3. This has been attempted several times with consequent severe hypothyroid symptoms before corrected with T4/T3 administration.
b. Also, since all red meat is red because of blood, which contains globulin-bound thyroid hormones (and other hormones), I urge marginal hypothyroid patients to increase their consumption of bloody red meats, raw or as rare as possible. (A short thought on supplementation: as omnivores and meat-eaters, we have a history of ingesting animals and their respective hormones; many of those hormones are the same as our own, particularly the thyroid hormones in mammals. Cooking is a relatively recent practice for hominids such as ourselves. I suggest that we developed as a species expecting at least some external sourcing of most of our blood-circulating hormones. De facto supplementation was occurring in our ancestor’s diets. Our endocrine glands may have developed over time expecting and even needing extrinsic hormone supplementation. Growl.)
c. A recent Japanese publication reports the detection of physiologically significant amounts of THYROXINE (T4) and LIOTHYRONINE (T3), as well as DIT and MIT in Laminaria sp. (Kombu) and Sargassum sp. (Sargasso Weed) (7). This has enormous implications regarding both dietary caution (for Kombu eaters) and for hypothyroidism treatments by healers. All seaweed health and nutrition studies using either Laminaria or Sargassum will need to be re-evaluated for the effects of probable cryptic T4 and T3 supplementation. Those who have been eating lots of Kombu regularly might wish to stop for 60-90 days and see if they become clinically hypothyroid. I strongly believe that many of the health benefits attributed to Kombu and other brown seaweeds are probably due to cryptic thyroid hormone supplementation. I refer to the lowering of arterial blood pressure, reducing blood triglyceride levels, promoting weight loss, resolution of skin problems, mood enhancement, etc. (7).
There seem to be no studies using either Kombu or Sargasso Weed to specifically treat any thyroid dysfunction. If the T4 and T3 in brown seaweeds is available from either eating dried uncooked powder or seaweed pieces, or eating lightly cooked seaweed as in Miso broth or fast stir fry, we may finally have a natural, non-animal source of actual thyroid hormones. Dosages and adverse signs will need to be established.
I recommend diagnosed low thyroid patients be given 2-5 grams of powdered Laminaria seaweed daily with close monitoring. The most probable first symptoms will be nervousness, sleep disruption, increased heart rate, heat intolerance, irritability.
This discovery of T4 and T3 in brown seaweeds supports my contention that we are an externally-sourced hormone-supplement-dependent species, whose historical uncooked omnivorous diet provided dietary sources of most mammalian hormones and that the lack of these hormones in our diets has made us less healthy, endocrine-deprived, and especially susceptible to absorbing toxic hormonal mimics.
8. In Hashimoto’s thyroiditis, immune modulation is suggested. The idea is to mitigate if not reverse the immune management decision to attack and possibly destroy the thyroid gland. I recommend the immunemodulating botanicals, particularly Ganoderma mushroom broth and tinctures of Ganoderma and Eleutherococcus.
9. Eliminate unnecessary X-rays to head and chest (dental, TB, CAT-scans, mammograms etc.)
10. Reduce exposure to potential thyroid hormone mimetics and confounders such as PCBs; polychlorinated biphenols resemble T4 and T3, which are biphenols, with their respective two aromatic rings. Especially try to reduce exposure to these and related substances for pregnant and nursing mothers and their young children. Many of the cryptic thyroid disruptions which act on the unborn and neonates may not manifest until primary years as psychiatric disturbances or as development disruption during puberty. (3)
11. There is an especially vicious class of endocrine disrupters that have become ubiquitous in our human environment. These substances have been used to improve our lives. They are: flame retardants, resorcinolbased glues, and MBTE gasoline additive s used to boost octane after tetra-ethyl lead was banned.
The flame retardants, Poly-bromated di-ethyl ethers, PBDE’s, were mandated for children’s pajamas, bedding, stuffed toys, etc.; they are also in motel/hotel bedding, curtains, carpeting (all wall-to-wall), and upholstered furniture. They are present in all water, soil, and air. They are especially concentrated in mammalian milk, in particular human mothers’ milk. They are thyrodisruptive and pass transdermally from clothing into infants and children. It is the regular 8-12 hour constant contact with a child’s epidermis, which allows the unavoidable slow accumulation of PBDE’s. They were mandated to stop fire deaths resulting from cigarette and other smokers setting fire to bedding after falling asleep with lighted smoking materials in hand. So, we are all secondarily poisoned by smoke even though we are miles from any known smoker. Not only does second-hand smoke kill, second hand protection from smokers is disrupting all of us.
Resorcinol and Dihydroxybenzene has been used therapeutically as an alleged starting molecule for catechols. Industrially, it is used in the production of Rayon and Nylon, and the superb resorcinol/formaldehyde glues, particularly in plywood, chipboard, and sawdust composites for fake wood furniture.
As these products are abraded, scuffed, cut, or broken, tiny amounts or resorcinol polymer dust particles are released into our living spaces and are inhaled, where they rest on mucous membrane surfaces where nano amounts are continually absorbed and may be thyrodisruptive. The EPA hearings on resorcinol were especially opaque and seemingly non-conclusive, in part, I suspect, because of the huge worldwide human exposure to resorcinol polymer fragments. The effects of resorcinol on the human thyroid are still being investigated.
I believe these resorcinolsourced particles may be a significant factor in the increasing thyroid epidemic, particularly in the countries where the most resorcinol has been used.
Gasoline additives are also being breathed by all of us. Many are thyrodisruptive.
REFERENCES
1. Bianco, A.C. Et Al. 2002. Biochemistry, Cellular Molecular Biology, and, Physiological Roles of the Iodothyronine Selenodeiodinases. Endocrine Reviews 23: 38-89
2. Budd, M. 2000. Why Am I So Tired? (Is Your Thyroid Making You Ill?)
3. Colburn, T. 2004. Neurodevelopment and endocrine disruption. Environmental Health Perspectives.112, 944- 949 3.A. Koppe, J. G. Are maternal antibodies generated by PCBs the missing link to impaired development of the brain? Ibid. 112:A682
4. Drum, R.W. 2000. Botanicals for Thyroid Function and Dysfunction: www.partnereartheducation.com
5. Gartner, R. et al. 2002 Selenium supplementation in patients with autoimmune thyroiditis decreases thyroid peroxidase antibodies concentrations. Jour. Clinical Endocrinology & Metabolism 87: 1687-1691
6. Greenspan, F>S> and Strewler, F>J> 1997. Basic and Clinical Endocrinology
7. Kazutosi, Nisizawa. 2002. Seaweeds Kaiso: Bountiful Harvest From the Seas. Sustenance for Health and Wellbeing.
8. Weiss, R. 1960(1996). Herbal Medicine (English translation)
9. Wichtl, M. and Bisset, H>G> 1994. Herbal Drugs and Pharmaceuticals
10. www.optimox.com