Thyroid dysfunction is epidemic in North America. One in ten adult American women have been diagnosed with thyroid disorders and some endocrinologists suggest that as many as 25% of adult American women are presenting with clinically detectable thyroid dysfunction. Health practitioners in Canada, Saudi Arabia, and Ireland (personal communication) report a similar apparent very startling increase in female thyroid disorders. Most veterinarians in small animal practice are seeing thyroid problems in cats and dogs balloon up to 40% of their respective practices (cats tend to be hyperthyroid and dogs tend to be hypothyroid; the proportional dosage for pets seems to be much higher for thyroid hormone treatments). What has happened?
Are practitioners finally becoming more aware of the many facets of thyroid function presentations?
Or, has something happened in the environment that is responsible for the apparent great increase in clinical and subclinical thyroid dysfunction? In clinical practice I am somewhat incredulous at the recent rapid increase in patients (90% female) presenting with both diagnosed and probable thyroid dysfunction (1995-2001). Just for a reality check, I went back to my old (1967) Robbins’ Pathology to see if he had anything to say about frequency of thyroid presentations. He did: “Diseases of the thyroid, while not common in clinical practice, are nonetheless of great importance because most are amenable to medical or surgical management.”
“Not common in clinial practice?”
Either people, practitioners, or the environment have changed, singly or perhaps in concert. I do not believe that Robbins was joking. His so hopeful prognosis for thyroid case management might bring bitter responses from the millions of women who have experienced surgical or radiation ablation removal of their thyroids only to have many or most of their presenting symptoms and others return with a vengeance. The patient help phone lines at the Thyroid Foundation of America are flooded with thousands of calls from women wondering, “how come I feel awful again?” Too often their endocrinologists dismiss their valid complaints as imagination or psychological character flaws. These mostly female patients are being very poorly managed from my viewpoint. Currently, TFA endocrinologists are actively trying to improve this situation (personal communication from L. Wood to R. Drum.)
Worldwide, thyroid dysfunction is a probable risk factor for 1 to 1.5 BILLION people (WHO figures) usually considered due to simple iodine deficiency and presenting as goiter (at least 200 million), complex mental retardation from fetal and neonate iodine deficiency (iodine deficiency causes more mental retardation worldwide than all other causes combined), and physical deformities (at least 20 million). The two main thyroid gland hormones are T4 (65% iodine) and T3 (59% iodine); calcitonin does not contain iodine.
The American thyroid dysfunction picture does not seem so simple: rather than simple iodine deficiency, it is the thyroid gland itself that seems to be failing. The claim has been made for almost 80 years that North Americans are getting plenty of dietary iodine due to the ubiquitous use of iodized salt. (Some Americans did not purchase iodized salt because it was a little more expensive, and plain salt was usually available nearby, often on the same shelf.) Braverman and others have even been suggesting that Americans are getting too much iodine and that increases in the incidence of autoimmune thyroid disease, namely Hashimoto’s Thyroiditis and Graves’ disease (hyperthyroidism) parallel increased dietary iodine intake, and that our high iodine intake, especially during the years 1940-1990, may be responsible for the thyroid dysfunction plague currently presenting. Recent surveys of food and alleged diets now indicate that the American diet may be borderline deficient in iodine intake, down from 5-800ug in l980 to about 135ug in 1995.
The truth is difficult to ascertain about any of these numbers, since no real people with real diets were followed very carefully by measuring iodine intake using precise analyses of iodine content in all food ingested per individual in the study population with concomitant precise measurement of urinary iodine for all urine secreted per 24 hours, for a few years; so, the authors merely fiddled and fudged and extrapolated until they had fallen prey to all of the traps of the SWAG syndrome. They just sort of guessed and pretended to be precise and then whined a lot about it at the expense of a lot of trees and tax dollars.
Until about a year ago, when I began to seriously read the materials and method sections of the original research papers on dietary iodine consumption, I truly believed all of these assumptions and conclusions. After reading the only paper (a British effort) that actually analyzed iodine content of a few foods and then extrapolated the rest, I learned that everyone else was just guesstimating with assumed academic authority. Too bad, it was such a great riff! For almost 60 years, the main dietary sources of iodine were not from iodized salt, but from flour products and dairy products. Iodates were/are used as dough conditioners; they improve the cross-linking in gluten molecules; they also act as mild antiseptics and mold retardants. The widely varying amounts of iodine in dairy products result from the use of copious amounts of iodine disinfectants used as teat dips in all commercial machine-milking dairy factories (hardly farms in either the traditional or realistic sense). The iodine solutions drip into the milk instead of large quantities of topical microbes. Furthermore, most dairy factories wash their stainless steel equipment with strong iodine solutions for sterilization. Do you ever wonder why you get a little hyperactive from eating cheese or drinking lots of milk?
People continue to get obvious low-iodine goiters even though the academics claim it is virtually impossible. The situation is much improved since the 1915-1919 years, when the number one cause of recruit rejection for military service was overt goiter. Low dietary iodine is associated with increased rates and risk for breast, endometrial, and ovarian cancer; the cause is probably gonadotropin stimulation with a resulting hyperestrogenic state characterized by relatively high production of estrogen and estradiol.
Now, I mention all of this because I personally believe that situational iodine deficiency regularly occurs in modern Americans as a result of both dietary peculiarities and the chronic use of fluoridated, chlorinated, and brominated water supplies, internally and externally. Fluorine, chlorine, and bromine are all more chemically reactive than iodine; when in the body, they all tend to disrupt stable iodine molecules, displacing the iodine and causing its excretion. When experimental rats (many dietary experiments are performed using volunteer incarcerates) are fed high-bromine diets, the bromine enters their respective thyroid glands and replaces the iodine already there; the proportion of bromine in the thyroid glands of those rats is directly proportional to the amount of bromine in their diet. We get bromine from pesticides, dough conditioners, and from disinfectants for water in hot tubs and commercial spas.
So, not only can we avoid eating iodized salt, we also can lose iodine from aggressive halides; our bodies have no known mechanisms for dealing with relatively large amounts of fluorides, chlorine, bromine, since these substances are normally too reactive to be available in the so-called natural environment; our exposure is totally modern. Gaseous chlorine is regularly released from shower and tub water freshly drawn from water supply taps. I recommend showering with the window open; I recommend bathing in tubs filled with the hottest water and allowed to out-gas while they cool to bearable temperature. Reduce your exposure to iodine-robbing halides for optimal thyroid health. Aspirin and other related salicylates as well as anticoagulants like Warfarin (dicoumerol) increase iodine excretion and can induce mild hypothyroidism; always ask mild hypothyroid patients about aspirin and anticoagulant use.
Where does iodine come from? It is mined in Oklahoma, Chile and Japan from subterranean brine deposits. How can we best get it into our diets and our bodies? No land plants are a good reliable source of iodine. Garlic grown near the sea often has relatively high amounts of biological iodine. Another peculiar phenomenon, biologically speaking, is the curious stuff called “snack foods”. These are extended shelf life products that cater to the most basic food desires of the economically deprived: greasy salty fried carbohydrates with lots of spoilage retardants and mystery ingredients euphemistically called “spices and other flavorings”.
The world’s largest snack food supplier, Frito-Lay, a division of PepsiCo, does not use iodized salt; presumably neither do any of the other snack food manufacturers, in part to reduce actual product production costs, but also with a wise eye to sloppy industrial mixing of potassium iodide in huge multi-ton batches of sodium chloride that has resulted in occasional pockets of nearly pure potassium iodide. Since both potassium and iodine are potentially deadly, this is a great potential source of ghastly liability. The hazard from Potassium poisoning is probably greater than from iodine: cardiac failure. Iodine would result in renal collapse. Usually excess iodine is simply excreted in the urine. Relatively huge amounts of iodine salts are used to serve as contrasting agents for radiography in the intestinal tract, up to 10 grams at once. (And these are the people that whine about eating a little kelp.) So, if your dietary sources of salt are largely from commercial foods, you might be iodine deficient. Iodized salt is approximately 0.01% potassium iodide; one teaspoon of iodized salt provides about 150ug of iodine, which, assuming 70-80ug intestinal uptake, is probably the real daily adult requirement.
For my patients, I prescribe daily dietary dosages of 3-5 grams of a good powdered kelp, which should provide enough iodine and most of the essential trace elements (4 grams of powdered seaweed per day is 1 ounce per week, is 3 and 1/4 pounds of seaweed per year.) Any seaweed contains more available dietary iodine than any land plant. The seaweeds with the most available iodine are the giant kelps of the northern hemisphere, with the highest concentrations of iodine occurring in the most northern kelps (8000 ppm in Icelandic kelp, 4000 ppm in Norwegian kelp, 1-2000 ppm in Maine and California kelp; the seaweeds with the least amounts of iodine are Nori, about 15ppm, and Sargassum, about 30-40 ppm). Besides garlic, root crops, vegetables such as turnips, carrots, potatoes, parsnips, sweet potatoes, and chocolate (actually, the iodine in chocolate probably originates as teat dip and transfers into the milk of milk chocolate). The amounts of iodine in land plants can be greatly increased by fertilizing food plants with seaweeds applied directly to the soil as topical mulch or tilled into the soil. I do not know if foliar sprays containing seaweed extracts provide iodine that is absorbed into edible plant parts.
There is one more terrible problem: the atomic age. Since 1945 every human has been repeatedly dusted with radioactive fallout (from both acknowledged and unacknowledged nuclear explosions), nuclear power plant disasters, and most insidious of all, the regular, continual, intentional release of radioactive Iodine 131 from all nuclear weapons facilities and all nuclear power plants with so-called normal operations.
In addition to this, the government-sponsored nuclear industry has regularly released enormous quantities of radioactive iodine, cesium, and strontium into the atmosphere just to see what might happen. Eastman Kodak was forewarned so they would not lose photoemulsion film to radioactive fogging. Families downwind of Hanford reservation in Washington were not warned. For nearly 5 years, a 100,000-page report prepared by the National Cancer Institute was suppressed until forced out of hiding by the efforts of some senators and congressmen, most notably Senator Tom Harkin of Iowa. The report shows total disregard for American citizens and military. Hundreds of thousands of delayed thyroid pathologies are the long-term heritage of this inexcusable outrage. I BELIEVE CONTINUAL AND REGULAR EXPOSURE TO INCIDENTAL IODINE 131 IS THE ORIGIN OF MOST CURRENT THYROID DISORDERS. The prescribed treatment would be cultural and political maturation. Seaweeds alone are not enough.
It takes about 18 minutes for all the blood in the body to pass through the thyroid gland; it is the most thoroughly vascularized of all the endocrine glands. Most of our respective bodies are iodine conservative. We can absorb it through our skin in minutes when painted on; I have also had participants demonstrate transdermal movement of iodine absorbed from clothing thru the skin. Iodine is easily absorbed from the intestines, with efficiencies of up to 98% in very low-iodine diets. The radioactive iodine we are all breathing and eating is released in bursts as a product of nuclear fission usually within legally allowable amounts; these allowed amounts are calculated on a per day basis rather than as high-amount bursts or episodes. This helps perpetuate the myth that the allowable releases are no health hazard. Wrong. The episodic rather than regular release of iodine-131 means we get big hits and then none at all, especially in milk and milk products.
The reason that iodine-131 is so dangerous is that it has a relatively short half-life of about 8 days; this means it has a radiogenic life of about 60 days, and then the amount remaining is probably biologically insignificant. Although this short half-life is touted as a good thing for iodine-131-treated patients and incidental accumulators of iodine-131, the short half-life means that most iodine-131 taken into the body will decay in the body rather than being excreted. Rather than occurring over a relatively long time, the short half-life means a lot of radioactive decay of iodine-131 occurs within the thyroid gland, releasing molecular-destructive gamma radiation to nearby cells. There is no safe dosage of gamma radiation inside cells.
Therapeutically, iodine-131 is fed to hyperthyroid patients to fry their thyroids with gamma radiation, released by radioactive decay of iodine-131; the patient handout claims that this is a totally safe procedure with no possible health hazards; on the other side of the handout patients are severely warned to not nurse their babies for 5 weeks, not to hold children and other loved ones close, to not share towels for a month or more. So much for totally safe!
Our bodies tend to be iodine aggressive in absorption and iodine conservative in excretion. If we are at all iodine deficient, we will readily take in radioactive iodine-131 and deposit it in our thyroid glands just as we do with non-radioactive iodine-127. If we have a full, ongoing whole-body complement of iodine-127, our bodies tend to not take up any iodine-131. This means that eating seaweeds regularly, especially the big northern kelps, will provide both dietary iodine and protection against the ongoing iodine-131 hazards and the next unplanned nuclear disaster.
The major health problems from the Chernobyl nuclear disaster on or about 26, April 1986 are all related to the huge and deliberately underreported releases of radioactive iodine-131 into the atmosphere and onto the soils, surface waters, plants, animals, and cities within 1000 miles of the Chernobyl site. Within five years, large increases in thyroid disorders of all sorts began to occur, directly attributable to Chernobyl iodine-131 releases. The worst is still developing since we know that the cancer rates from short-term radiation exposure tend to peak 20-30 years after a particular release episode. The simplest protection against nuclear fallout is to simply dismantle all nuclear facilities immediately. Without that, we are all continually at risk for thyroid dysfunction. Our next best protection against thyroid disruption is to body-load with iodine contained in iodine-rich whole raw seaweeds as regular daily consumption. If our bodies have an ongoing full complement of iodine-127, we can better resist taking in incidental iodine-131.
There are a few more little bits to the iodine part of the story: After the thyroid gland, the distal portions of the human mammary glands are the heaviest users/concentrators of iodine in tissue. Iodine is readily incorporated into the tissues surrounding the mammary nipples and is essential for the maintenance of healthy functioning breast tissue. I suspect that this is ignored in the attempts to understand the developmental dynamics of breast cancer; I believe that radioactive decay of iodine-131 in breast tissue is a significant factor in the initiation and progression of both breast cancer and some types of breast nodules. Iodine also concentrates in the salivary glands and gonads. Salivary gland cancer, and testicular cancer (especially in men over 25, a relatively recent phenomenon) and ovarian cancer are all increasing in actual numbers. I suspect that radioactive iodine-131 decay may be a significant contributing factor.
The largest of the endocrine glands, the one-half to one ounce thyroid gland is almost twice as large in women, on average, than in men. Its overt function seems to be to manufacture, store, and release, under strict controls, thyroid hormones, mostly thyroxin, T4, and T3, tri-iodothyronine, in about a 4:1 ration. In very low iodine intake situations, that T4:T3 ratio is reversed to 1:4. This rather comfortable view of the mechanistic thyroid is incomplete: to quote Robbins (Pathology, 1967) further, “from the physiologic standpoint, the thyroid gland is one of the most sensitive organs in the body. It responds to many stimuli and IS IN A CONSTANT STATE OF ADAPTATION…. During puberty, pregnancy, and PHYSIOLOGIC STRESS FROM ANY SOURCE, THE THYROID GLAND INCREASES IN SIZE AND BECOMES MORE ACTIVE FUNCTIONALLY. Changes in size and activity may be observed during a normal menstrual cycle. This extreme functional changeability is manifest as transient hyperplasia of thyroidal epithelium (follicular cells) changing (to tall, columnar). When stress abates, involution obtains and normal follicular cell shape (roughly spherical) and function resume”. Instead of simply being a passive hormone factory, the thyroid gland overtly changes size, shape and function to reflect the changing reality of its particular person.
Patients and workshop participants regularly provide real anecdotal evidence (I usually give more credence to a person’s evaluation of their own experience than I do to the numbers coming out of dead machines; remembering that all information is technically anecdotal, all machines are innately unreliable, data are usually massaged, and scientists are no less biased or prone to lying than the general population) about the apparently frequent overmedication with thyroid hormone replacement medications: namely, that they stopped taking their thyroid medications when they started to feel worse after several months or years, and they not only felt better, but their symptoms never returned. The joyful cynic can reasonably claim that the thyroid replacement hormone medication(s) worked. Sometimes yes and sometimes no, is my evaluation of the situation. I believe that brief thyroid hormone replacement therapy may be life-saving and or life-modulating; but, I also think that the increasing reliance on TSH tests and the aggressive attempts to normalize the thyroid gland and its functions of a particular patient may mask the greater need which is to understand what is the gain to the patient from a change in thyroid function.
The other point, often dismissed now, is the full frontal location of the thyroid gland, with no bony protection on the anterior side unless head drop occurs. When I see the same patients over several years, modest changes in their respective thyroid size and sometimes shape are often evident, and resolve with no overt intervention. Unresolvable or otherwise overwhelming life situation stress often seems to be if not an initiating factor, at least an accompanying reality for benign thyroid enlargement. I am not yet clear from physiologic studies if nonpathological increased thyroid size is always accompanied by an increase in thyroid hormone production or release, or not. One interesting point is that impact trauma can apparently squeeze a burst of thyroid hormone out of the gland with a concomitant transient hyperthyroidism episode; this means a physical hit, or a compression squeeze from poorly placed shoulder belts in automobiles where the vehicle has been hit or has hit something and a whiplash event occurs. So, mechanical stress can also affect the thyroid gland. Many endocrine changes occur in anorexia nervosa, including low levels of T4 and T3.
I further believe that the situational low thyroid presentations (hypothyroidism) which seem to be initiated by a known life trauma (particularly loss of a loved one or similar grief-inducing events) are completely normal thyroid responses and very desirable components of the grief response and should not be treated unless acute (life-threatening), or persisting for more than one year. I believe that it is a failing of the cultural terrain that we do not honor and savor the natural grief response, with the personal consequence that many of us suffer from chronic secondary grief over the loss of therapeutic grieving and that this secondary grief is a major factor in the current plague of hypothyroidism.
Other tissues in the body, particularly the liver, can greatly influence the accessibility of T4 to body cells; for T4 to be physiologically active, it must first be converted to T3. This conversion is accomplished primarily by 5-deiodinase in the liver. Of intriguing interest, this particular enzyme requires selenium as its cationic enzymatic cofactor. This means that chronic selenium deficiency can present as hypothyroidism due to reduced T4 to T3 conversion. The thyroid test for TSH and T4 will not reveal this and unnecessary thyroid medication may be prescribed. In an associated consideration, mercury in the body tends to quell or cripple selenium in enzymes. This means that chronic (or even possibly acute) mercury poisoning can present as hypothyroidism. We all have steadily increasing body burdens of mercury from both our foods and water. A test for selenium and mercury is always indicated in cases of obvious hypothyroid signs and symptoms with normal range TSH and T4.
Recently I have read that isoflavones, such as genistein and equol, are inhibitors of thyroid peroxidase, the thyroid follicle enzyme that makes T4 and T3. This inhibition may generate goiters, hypothyroidism, and autoimmune thyroiditis. Since isoflavones are being touted as cancer preventatives, especially for breast and prostate cancers, their addition to non-soya foods may be a potential thyroid disaster. Isoflavones already available in soya foods may depress thyroid function through TPO inhibition.
Another almost bizarre phenomenon is the RT3 situation. RT3 is also called reverse T3. It is not reversed at all but instead is produced when the 5-iodine on the interior benzene ring is removed by 5-deiodinase, instead of the 5-iodine on the exterior site. RT3 is nearly inert and especially so as a thyroid hormone. It has an extremely short half-life in the body of a few hours; it is rapidly excreted via the liver. Normally, about 40% of the T4 in our bodies converts to T3 and about 45% converts to RT3. This is most curious in an otherwise innately metabolically conservative biological system. The RT3 mechanism is a way of regulating T3 and reducing the likelihood of incipient hyperthyroidism, whilst maintaining the capacity to boost T3 production as a situation may demand. The body can also decrease T3 production on demand: fasting, acute trauma, chronic illness, and grief all tend to increase RT3 production and decrease T3 production. A decrease in T3 tends to mean a slower metabolism, less appetite, slower protein replacement and much less energy on demand for spontaneous kinetics. A relatively high RT3 and low T3 is often accompanied by a relatively low body temperature (less than 97.5 degrees F) as measured in the axillaries before rising in the morning; this low armpit temperature reading (one assumes carefully calibrated and accurate mercury thermometers only being used) is often used as a simple test for hypothyroidism, since body temperature is tightly controlled by metabolic rate and metabolic rate (the rate at which fuel is converted to heat and kinetics) is controlled by T3. A shortage of T3 means lower body temperature (and possibly death if prolonged). The relatively high production of RT3 compared to T3 is sometimes referred to as Wilson’s Syndrome, and is clinically treated with T3 until a normal body temperature is “captured” and maintained.
There is not yet a positive consensus about either the efficacy or desirability of T3 therapy. I tend to think it is indicated in life-threatening situations and maybe in other cases. I believe that temporary low body resting temperature and accompanying low T3 may indicate physiological grieving and/or the need to slow down, get quiet, meditate, rest, regroup one’s life resources, and correct faulty attitudes or behaviors to more healthpositive ones. In the trauma response, low T3 and high RT3 function to keep the body still and unavoidably calm to slow or prevent further trauma thru activity. I think that up to a year of prolonged low T3 and or low T4 production might be a genetically programmed requirement for health renewal in a long-lived primate such as ourselves (remember that chimpanzees have lived well past 65 years in captivity) so that we can remain healthy for up to 120 years.
There is a sad note to the increasing clinical thyroid plague: between 2 and 8 million North Americans (the exact numbers will never be known due to poor record-keeping) were deliberately medically treated with Xrays to the head and chest, foolishly and often frivolously for a wide range of presenting conditions. These conditions included: scalp ringworm, asthma, chronic bronchitis, tonsillitis, acne, and neonate respiratory problems. The thyroid glands of these patients received pathologically significant amounts of powerful ionizing radiation. These treatments (occurring between 1930 and 1980) have caused over 10,000 of cases of thyroid cancers, which develop 10-40 YEARS after the medical exposures with a peak incidence between 20-30 years after the episodes, and as much as a million cases of other thyroid structural deformities including nodular goiters (at least 27% of all children and adolescents irradiated). Who was punished for this gross instance of medical malpractice? By the 1930’s the connection between cancer and radium exposure was known. The endocrinologists are relatively mum about responsibility for these poor trusting victims, more than the total number of victims wounded by the two atom bombs dropped on Japan in 1945.
If you have a person born before 1980 (most will be over 30 years old since the practice of sloppy upper body and head irradiation was largely discontinued by 1970 but persisted in some remote clinics and offices for up to another decade.), who presents with nodular goiter or thyroid cancer, be sure and inquire about juvenile radiation exposure. Treatment prognosis is mixed, with thyroidectomy usually recommended, with subsequent lifelong obligatory thyroid replacement therapy.
SEAWEED THYROID TREATMENTS
The complexity of many presenting thyroid dysfunction cases precludes a simple set of all-purpose formulas. Each one of my thyroid patients has a personally unique thyroid presentation. I try to compose an individualized functional treatment plan for each, using a few basic methods. Diet and behavior modification also are very important in thyroid case management.
What follows are some of my treatment approaches and some general guidelines and notes:
1. Rather uncomplicated seaweed therapy seems to help relieve many of the presenting symptoms of thyroid dysfunction. Some of the results are very likely from whole body remineralization (especially potassium, zinc, calcium, magnesium, manganese, chromium, selenium, vanadium etc.) in addition to thyroid gland aid from both sustained regular reliable dietary sources of biomolecular iodine and from thyroxin-like molecules present in marine algae, both the large edible seaweeds and their almost ubiquitous epiphytic microalgae, predominantly the silica-walled diatoms. Seaweeds provide ample supplies of most of the essential trace elements required for adequate enzyme functioning throughout the body but especially in the liver and endocrine glands.
2. Regular biomolecular seaweed iodine consumption is more than just thyroid food: it can also protect the thyroid gland from potential resident iodine-131-induced molecular disruption and cell death when the thyroid gland is fully iodized with iodine-127. The fear of eating seaweed because it might be contaminated with iodine-131 is easily mitigated by allowing the seaweed to be stored for 50 days prior to consumption; this will give enough time for most (99%) of any Iodine-131 to radioactively decay. A simple folk test for iodine deficiency or at least aggressive iodine uptake, is to paint a 2 inch diameter round patch of USP Tincture of Iodine (strong or mild) on a soft skin area such as the inner upper arm, the inside of the elbow, the inner thigh, or the lateral abdomen between the lowest rib and the top of the hip. If you are iodine deficient, the patch will disappear in less than two hours, sometimes as quickly as 20 minutes; if it fades in 2-4 hours, you may just be momentarily iodine needy. If it persists for more than 4 hours, you are probably iodine sufficient. (This test is of course easier to use with Caucasians and may not offer sufficient color contrast in brown-skinned people.) Iodine deficiency seems to predispose people to thyroid malignancy; this could explain the apparent thyroid cancer distribution “fans” downwind of nuclear facilities in previous goiter belt areas.
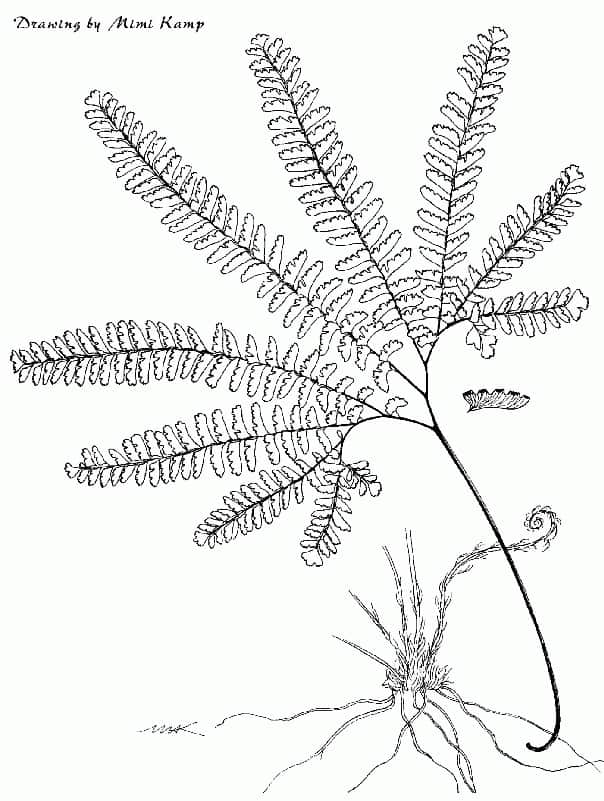
3. Many patients with underactive thyroid glands complain of a sense of “coldness” or feeling cold all of the time; often they are overdressed for warmth (by thyro-normal people’s standards). They may also present a low basal body resting temperature, as measured by taking their armpit temperature before rising in the morning (remember to shake down the thermometer the night before). Other symptoms may include sluggishness, gradual weight gain, and mild depression. For these patients, add 5-10 grams of several different whole seaweeds to the daily diet; that is, 5-10 grams total weight per day, NOT 5-10 grams of each kind of seaweed. I usually suggest a mix of 2 parts brown algae (all kelps, Fucus, Sargassum, Hijiki) to one part red seaweed (Dulse, Nori, Irish moss, Gracillaria). The mixed seaweeds can be eaten in soups, salads, or powdered and sprinkled onto or into any food. I recommend doing this for at least 60 days, about two lunar cycles or at least two menstrual cycles; watch for any changes in signs and symptoms and any change in average daily basal temperature. (Please note that patients can have a normal 98.6 degree F temperature and still feel cold, and, also present many of the signs and symptoms of functional hypothyroidism.)
Please do not insist that all hypothyroid patients must have abnormally low basal resting temperatures. If no symptoms improve or the temperature remains low (less than 97.5 degrees F), continue seaweeds and request a TSH and T4 test. If TSH and T4 tests indicate low circulating thyroxin levels, continue seaweeds for another two months. It may take their thyroids that long to positively respond to continual presentation of adequate dietary iodine. Powdered whole seaweed may be much more effective than flakes, pieces, or granules. The powdered seaweed is best added to food immediately prior to eating; do not cook the seaweed for best results. All corticosteroids tend to depress thyroid function. Before trying to fix the thyroid, be sure to aggressively inquire about both internal and topical steroid use, including Prednisone and topical creams. Salicylates and anticoagulants can also aggravate existing mild hypothyroidism.
4. Partial thyroidectomy cases can be helped by regular continual dietary consumption of 3-5 grams of whole seaweeds 3-4 times a week. By “whole seaweed” I mean: untreated raw dried seaweed, in pieces or powder, not reconstructed flakes or granules.
5. Patients with thyroid glands on thyroid replacement hormone (animal or synthetic) can respond favorably to carefully and slowly replacing part or all of their entire extrinsic hormone requirement by adding dietary Fucus in 3-5 gram daily doses. Fucus spp. has been the thyroid folk remedy of choice for at least 5000 years. The best candidates are women who seek a less hazardous treatment than synthetic hormone (after reading that prolonged use of synthetic thyroid hormone increases risk for heart disease, osteoporosis, and adverse interactions with many prescribed drugs, particularly corticosteroids and antidepressants).
Fucus spp. contain di-iodotyrosine (iodogogoric acid) or DIT. Two DIT molecules are coupled in the follicular lumina of the thyroid gland by a condensing esterification reaction organized by thyroid peroxidase (TPO). This means that Fucus provides easy-to use-prefabricated thyroxine (T4) halves for a boost to weary thyroid glands, almost as good as T4. European thalassotherapists claim that hot Fucus seaweed baths in seawater provide transdermal iodine; perhaps hot Fucus baths also provide transdermal DIT?
The best results with Fucus therapy are obtained with women who were diagnosed with sluggish thyroid glands and who are (or were) on low or minimal maintenance replacement hormone dosages and who may gleefully remark that they miss, forget, or avoid taking their thyroid medication for several days with no obvious negative short-term sequelae; others claim to have just stopped taking their medication. I do not recommend stopping thyroid medication totally at once: Thyroxin is essential for human life (and all animal life); it has a long halflife in the body of a week or more, so a false impression of non-dependency can be obtained for up to two months before severe or even acute hypothyroidism can manifest, potentially fatal.
Even though I personally do not recommend it, women regularly just stop taking their thyroid replacement hormone, even after years of regularly and faithfully taking their medication. In many cases their thyroid glands resume thyroxine production after a 2-3 month lag time with many of the signs and symptoms of hypothyroidism presenting while their thyroid glands move out of inactivity. IT IS IMPERATIVE TO UNDERSTAND THAT THIS COMPLETE CESSATION OF TAKING THYROID REPLACEMENT CAN ONLY BE SUCCESSFUL IN PATIENTS WHO HAVE A POTENTIALLY FUNCTIONING THYROID GLAND. Those who have had surgical or radiation removal of their respective thyroid glands must take thyroid hormone medication containing thyroxine to stay alive.
Fucus can be easily added to the diet as small pieces, powdered Fucus in capsules, or freeze-dried powder in capsules. The actual Fucus is much more effective than extracts. A nice note is that Fucus spp. are the most abundant intertidal brown seaweeds in the northern hemisphere. This is of especial interest to those patients who might be trading one dependency for another, as seems to be the case for some. (A year’s supply can be gathered in an hour or less and easily dried in a food dehydrator or in hot sun for 10-12 hours and then in a food dehydrator until completely crunchy dry. Fucus dries down about 6 to one: six pounds of wet Fucus dry down to about one pound. It has a modest storage life of 8-12 months in completely airtight containers stored in the dark at 50 degrees F. A year’s supply at 4 grams/day is slightly more than three pounds dry).
6. Aggressive attempts to replace thyroid replacement hormone with Fucus involve halving the dose of medication each week for four weeks while adding 3-5 grams of dried Fucus to the diet daily from the beginning and continuing indefinitely. If low thyroid symptoms appear, return to the lowest thyroid hormone maintenance level and try skipping medication every other day for a week, then for every other two days, then three days, etc. The intent is to establish the lowest possible maintenance dosage by patient self-evaluation and/or to determine if replacement hormones can be eliminated when the patient ingests a regular reliable supply of both biomolecular iodine and DIT. Thoughtful, careful patient self-monitoring is essential for successful treatment.
7. A more conservative replacement schedule is similar to the aggressive approach except that the time intervals are one month instead of one week, and the Fucus addition is in one gram increments, beginning with one gram of Fucus the first month of attempting to halve the replacement hormone dosage, and increasing the amount of Fucus by a gram each succeeding month to 5 grams per day. The conservative schedule is urged with anxious patients and primary caregivers.
There is some literature concern (a bit quite shrill and clumsily documented) that excess (undefined) kelp (species either unknown or not mentioned) consumption can/may induce hypothyroidism. It seems possible. The likely explanation is an individual’s extreme sensitivity to dietary iodine; Icelandic Kelp (a Laminaria sp.) can contain up to 8000 ppm of iodine; Norwegian kelp can contain up to 4000 ppm of iodine. Most “kelps” contain 500-1500 ppm of iodine. Nori has about 15 ppm of iodine.
The only definitive study I have seen reports from Hokkaido, Japan, where study subjects, at about an 8-10% rate of total study participants, presented with iodine-induced goiter from the consumption of large amounts of one or more Laminaria species (Kombu), known to be rich (more than 1000 ppm) in available iodine. Reduction of both total dietary iodine and/or dietary Kombu led to complete remission of all goiters. The apparent iodineinduced goiters did not affect normal thyroid functioning in any participants. Two women in the study did not care if they had goiters and refused to reduce their Kombu intake. Note that the Japanese have the world’s highest known dietary intakes of both sea vegetables and iodine.
I think the reduction or elimination of seaweeds from the diet is indicated for at least a month in cases of both hyperthyroidism and hypothyroidism, to ascertain if excess dietary iodine is a contributing factor to a disease condition. Other dietary iodine sources, particularly dairy and flour products should also be reduced and or eliminated during the same time period. Some individuals do seem to be very dietarily iodine-extraction efficient and iodine sensitive simultaneously.
BRIEF CASE HISTORY OF A THYROID NODULE
A 35-year-old female patient (two children) presented with a rapidly growing thyroid nodule that seemed to arise with no overt cause. The nodule was not firm but cystic. Once it had stabilized, a fine needle aspirant sample was collected; the cyst was apparently totally benign. Synthetic thyroid hormone was suggested to promote the nodule’s shrinkage. The patient refused. Almost four years after the nodule stabilized the woman began taking 3-5 grams/day of powdered Fucus and Nereocystis kelp, mixed. After six months, the nodule had completely disappeared. The woman continues to take some maintenance dosages several times a week.
OTHER HERBAL THYROID TREATMENTS
Graves Disease; Hyperthyroidism
Unlike Hashimoto’s Thyroiditis, Graves’ Disease seems very amenable to successful herbal intervention and control. The three main herbs used are: Melissa officinalis (Lemon Balm), Lycopus virginicus (Bugleweed) and Leonurus cardiaca (Motherwort) in descending order of strength and apparent thyrosuppressive efficacy.
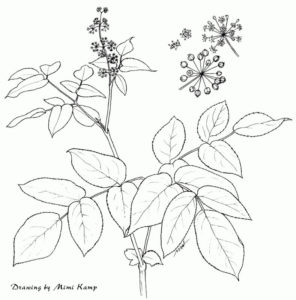
Melissa officinalis (Lemon Balm) in particular, when delivered in measured doses as tincture, tea, or less exactly, freshly extracted juice from a “wheatgrass juicer” stops TSH from binding to its thyroid receptor sites, slows or even quells the uptake of iodine by the active transport sites on thyroid cell surfaces, suppresses the iodination of tyrosine residues in the follicular lumina by TPO, and appears to also impede stored thyroid hormone release from the thyroid gland. The results can be especially rewarding (see following case history). My personal preference is to have hyperthyroid patients grow and harvest their own Melissa, and also to prepare their own medicine. Melissa grows abundantly in all except xeric habitats with sufficient water and a little shade. It will overwinter in pots. The freshly expressed juice can be frozen. I do not know if freeze-dried Melissa products are effective.
A critical point for herbal treatment of Graves’ is the active and aware participation of the patient in monitoring both symptoms and their respective body responses to herbal treatment. Melissa has a fine reputation as a calming herb and it may be that the calming action is not as a nervine, but as a very effective thyrosuppressant. I do not have data on the proportions of T4:T3, or T3: RT3 in Melissa treatment of Graves’. The possibility of potential overmedication with Melissa, a temporary hypothyroidism, exists, but I have no known cases to report.
Lycopus spp. (Bugleweed) Apparently both the American species and the European one are effective in slowing down TSH adherence to its rightful cell surface receptors and the uptake of iodine by thyroid cells. It does not seem as quick as Melissa.
Ruth Dreier, one of my former apprentices, reported in the 1994 Journal of the Northeast Herbal Association about her long and arduous but eventually successful efforts to slow and stop progressive Graves’ using tea, tincture, and fresh plant material of Lycopus virginicus. She found the tea and tincture to be more effective than the fresh plant material, which suggests to me that some type of molecular cleavage or rearrangement is necessary for effective use of Lycopus as a thyrosuppressive. She also used severe dietary restrictions and careful self-monitoring of her symptoms, using the tincture as a sort of quick fix medication.
Leonurus cardiaca (Motherwort) I do not have direct experience with Leonurus as a thyrosuppressive. Some of its purported almost narcotic effects as a somnambulant may be due to thyrosuppressive activity.
A cautionary note: Persons with undiagnosed Graves’ Disease may become hyperthyroid from absorption of increased dietary or topical iodine.
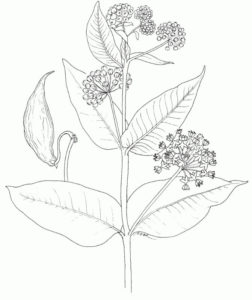
Oplopanax horridum (Devil’s Club) Contemporary British Columbia coastal natives drink a strong tea (decoction) of Oplopanax root and stem bark to allegedly cure hyperthyroidism (see: Turner, N, as ref. in Three Herbs). I do not know the dosages or the duration of the treatment. I predict that a correlation exists between Oplopanax’s type II diabetes remediation and its successful thyrosuppression. The post-consumption Oplopanax lethargy may be thyrosuppression at the TRH hypothalamic level rather than direct action on the thyroid gland.
A BRIEF CASE HISTORY OF GRAVES’ DISEASE
A 47 year old female was diagnosed with Graves’ disease based on blood tests ordered by an endocrinologist she had been referred to by her family doctor. She was first alerted to the likelihood of thyroid dysfunction by her pedicurist, who noted the recently greatly thickened skin on her feet. The patient also presented feeling hot all of the time, increased sweating, heat intolerance, insomnia, huge appetite, hyperactivity, fatigue, heart palpitations, manual tremor, and eye irritation, all Graves’ hyperthyroid symptoms. Her tests were TSH < 0.03 (normal range is 0.5-3.5) and T4 224 (normal range 65-165). A family health and emotional crisis had generated acute worry and anxiety.
The endocrinologist offered her three therapeutic choices: Surgical thyroid gland removal, use of thyrosuppressive drugs, or using radioactive iodine to burn the thyroid gland out of existence. None of these were acceptable, so she went to see a naturopath/acupuncturist and began taking tinctures of Bugleweed, Siberian Ginseng, Motherwort, Lemon Balm, and, a bit later, Hawthorn in addition to acupuncture treatments. In five months her T4 had declined a bit to 198, but her TSH remained essentially nothing at <0.03. She started a homeopathic constitutional remedy (Pulsatilla 30x). A few weeks later I recommended she begin taking a green drink of freshly blended Lemon Balm (Melissa officinalis) in daily doses of 2-3 liquid ounces with food in addition to her tinctures and homeopathic remedy. In three months her T4 was 50% lower at 113, but her TSH was still <0.03. She continued the treatment plan for another 5 months until her THS and T4 were in the normal range. She stopped all herbs and the homeopathic remedy, and her endocrinologist declared her cured. WITHOUT THYROIDECTOMY BY SURGERY, RADIOACTIVE ABLATION, OR STRONG ANTITHYROID DRUGS. (There is a significant risk increase for women who use thyrosuppressive drugs for hip fracture).
A few more notes:
Maude Grieve, in her extensive section on Nettles, discusses somewhat cryptically the use of powdered nettle seeds as a treatment for goiter. No easy access to corroborating references or a case history (which was not her task). I know of only one anecdotal report where a young woman claimed to have cured her goiter with nettle seeds. May bear investigating. It was not at all clear as to what type(s) of goiter were treated.
Hypothyroidism does not respond to any particular herbs that I know of, in either a hopeful or remedial manner. Seaweed therapy with a strong fresh green vegetable diet, particularly chickweed, dandelion, parsley, spinach, and beet greens, seems to be the best. Brassicas are probably best kept to a minimum because of their known goitrogenic activity.
Further dietary comments: I usually recommend eating very little or no flour products in an effort to reduce erratic iodine intake and to reduce bromine intake as well as reduce the hyperglycemia that often accompanies the eating of flour products and simple sugars (I also recommend totally eliminating all simple sugars except fresh fruit). All non-organic meat and meat products are contraindicated since xenoestrogens can disrupt thyroid function (just like intrinsic estrogens generated by the patient’s body). I usually suggest elimination of all dairy products except unsalted organic butter to further reduce exposure to growth hormones and iodine and unwanted tetracycline residues. I usually recommend eating avocados, organic eggs, and sardines to provide quality fats to keep that bile flowing and wasted thyroid hormones moving out of the liver.
DIETARY BLOOD AND BLOOD PRODUCTS
All blood will contain some thyroid binding globulin-bound thyroid hormone. The consumption of red meat will always provide small but significant sources of extrinsic thyroid hormone and, at the least, some dietary iodine. In areas of endemic goiter (continental Eurasia), blood products such as blood sausage were regularly consumed. The blood from slaughtered animals was carefully caught when the animals were bled. Blood pudding and blood sausages are still regularly served in traditional Irish Breakfasts and are regularly available in meat shops throughout Great Britain and the European Union countries as well as in eastern Europe. Blood pudding and blood sausage are folk treatments for fatigue and sluggishness. I assume that T4 is the most active constituent after iron.
In his privately published memoir, Of Desert Plants and Peoples, Sam Hicks writes about the use of fresh deer blood by indigenous peoples in the Sonoran Desert to treat what reads like hypothyroidism. The dosages were about a pint or more of fresh deer blood biweekly or monthly. Just about right for time-release T4. For hypothyroid meat-eating patients, I definitely prescribe bloody organic meat and organic blood sausage; or, blood can be caught from home-grown and slaughtered animals known to have no growth hormones or pesticide exposure.
BIBLIOGRAPHY AND SEA VEGETABLE SOURCES
Arem, Ridha, The Thyroid Solution, 1999
Arnes, B. & Galton, L., Hypothyroidism: The Unsuspected Illness, 1976
Bergner, P., The Healing Power of Minerals, 1997
Budd, M., Why Am I So Tired? 2000 (Thorsons)
Colburn, T., Dumanoski, D., and Myers, J., Our Stolen Future 1996
Ditkoff, B. and Lo Gerfo, P., The Thyroid Guide 2000
Grieve, Mrs. M., A Modern Herbal. v. 2, 1931 (1971 Dover Reprint) p. 578
Greenspan, F.S. & Strewler, F. J., Basic and Clinical Endocrinology, 1997
Hamburger, J., The Thyroid Gland, Suite 303, 29877 Telegraph Rd., Southfield, MI 48034
National Women’s Health Report 22: #5, Oct. 2000. Thyroid Disorders and Women’s Health 1-877-986-9472
Oschman, J. L., ENERGY MEDICINE: The Scientific Basis, 2000
Pert, C., The Molecules of Emotion, 1997
Pert, C, Dreher, X., & Ruff, M., “The Psychosomatic Network: Foundations of Mind-Body Medicine”,
Alternative Therapies 4 (4): 30-41, 1998
Robbins, S., Pathology, 1967
Rosenthal, S., The Thyroid Sourcebook, 1996
Schecter, S., Fighting Radiation and Chemical Pollutants, 1997
Shannon, S., Diet for the Atomic Age, 1993.
Shomon, M., Living Well With Hypothyroidism, 2000 (Avon)
Surks, Martin, The Thyroid Book, 1999 (Self-published)
Thyroidnews@onelist.com; online thyroid resources
Wichtl, M. & Bissett, H.G., Herbal Drugs & Pharmaceuticals, 1994. Pgs. 329-332.
Wilson, Dennis, A Doctor’s Manual for Wilson’s Syndrome, 1995. 1-800-621-7006
Wood, L. C., Cooper, D.S., & Ridgway, E.C., Your Thyroid, 1995. The best easy to read thyroid book. Doctorbiased and patronizing.
THYROID PATIENT SUPPORT ORGANIZATIONS
• American Foundation of Thyroid Patients (281) 855-6608; 18534 N. Lyford, Katy, TX 77449
• American Thyroid Association (904) 353-7878; www.thyroid.org Email: admin@thyroid.org
• National Graves’ Disease Foundation (704) 877-5251; 2 Tsitsi Ct., Brevard, NC 28712
• Thyroid Cancer Survivor’s Association (877) 588-7904; POB 1545, NY, NY 10159-1545
• Thyroid Foundation of America (800) 832-8321; 410 Stuart St. Boston, MA 02116-2698